Indian Dental Association (IDA) is India’s leading advocate for oral health for the public at large. The association advocates that all Indians deserve good dental health because ‘healthy teeth and gums aren’t a luxury, they’re essential to general health and well-being’. Hence IDA launched the National Oral Health Programme (NOHP) comprising of a number of initiatives to make a difference nationwide and create a movement aimed at ending the oral health crisis faced by Indians today.
Oral health is vital to overall health and wellness for people of all ages, from infancy through adulthood. Indian Dental Association in the 21st century, is committed to providing all Indians with high quality, affordable, and accessible oral health care. It is clear that achieving health and oral well being requires a broad and collaborative approach which translates into IDA helping dentists succeed and advance the oral health of the public. After all, our members shape the future of this profession and IDA.
We accepted the challenge to improve overall health by initiating effective programs on oral health promotion and disease prevention by formulating and promoting the establishment of National Oral Health Policy, assisting state oral programs for the prevention of oral diseases; strengthing professionals' knowledge and skills; provision of information on oral health to health officials and policymakers, conducting conferences on public oral health and organizing special events for the public to educate and influence their oral health habits.
The goal is to help all Indians attain best oral health by addressing the oral health crisis in three distinct areas:
- Provide care to people who do not have access to oral health care.
- Strengthen and expand the public / private safety net.
- Disease prevention and Oral Health Education.
IDA serves as a catalyst for uniting Dental Professionals and organizations raising a powerful voice against the silence, to make a difference through ‘wake-up call’ for provision of better oral health. It called upon policymakers, community leaders, private industry, health professionals, the media, and the public to affirm that oral health is essential to general health and well-being and to take action. No one should suffer from oral diseases or conditions that can be effectively prevented and treated.
Taking good care of your mouth, teeth and gums is a worthy goal in itself. Good oral and dental hygiene can help prevent bad breath, tooth decay, and gum disease — and can help you keep your teeth throughout life.
A healthy mouth may help you ward off medical disorders. The flip side? An unhealthy mouth, especially if you have gum disease, may increase your risk of serious health problems such as heart attack, stroke, poorly controlled diabetes and preterm labor.
To understand the importance of oral health; its connection to your overall health is necessary.
In a word, plenty. Visual examination or a swab of saliva can tell your doctor volumes about your general health.
Your mouth is a window to the rest of your body. It often serves as a helpful vantage point for detecting the early signs and symptoms of systemic disease — a disease that affects or pertains to your entire body, not just one of its parts. Systemic conditions such as AIDS or diabetes, for example, often first become apparent as mouth lesions or other oral problems. In fact, according to the Academy of General Dentistry, more than 90 percent of all systemic diseases produce oral signs and symptoms.
Saliva contains antibodies that attack viral pathogens. It contains proteins called histatins, which inhibit the growth of a naturally occurring fungus called Candida albicans. When these proteins are weakened by HIV infection or other illness, candida can grow out of control, resulting in a fungal infection called oral thrush.
In fact, the ability to detect HIV-specific antibodies has led to the production of commercial, easy-to-use saliva test kits. In the future, saliva testing may replace blood testing as a means of diagnosing and monitoring diseases such as diabetes, Parkinson's disease, cirrhosis of the liver and many infectious diseases.
Saliva also protects you against disease-causing bacteria. It contains enzymes that destroy bacteria in different ways, by degrading bacterial membranes, inhibiting the growth and metabolism of certain bacteria, and disrupting vital bacterial enzyme systems.
Though your saliva helps protect you against some invaders, it can't always do the job. More than 500 species of bacteria thrive in your mouth at any given time. These bacteria constantly form Dental plaque — a sticky, colorless film that can cling to your teeth and cause health problems.
Long-term gum infection can eventually result in the loss of your teeth. Recent research suggests that there may be an association between oral infections — primarily gum infections — and poorly controlled diabetes, cardiovascular disease and preterm birth. More research is needed to determine whether oral infections actually cause these conditions, which include:
- Poorly controlled diabetes. If you have diabetes, you're already at increased risk of developing gum disease. But chronic gum disease may, in fact, make diabetes more difficult to control, as well. Infection may cause insulin resistance, which disrupts blood sugar control.
- Cardiovascular disease. Oral inflammation due to bacteria (gingivitis) may also play a role in clogged arteries and blood clots. The bacteria in the mouth may cause inflammation throughout the body, including the arteries. This inflammation may serve as a base for the development of atherosclerotic plaques in the arteries, possibly increasing your risk of a heart attack or stroke.
- Preterm birth. Severe gum disease may increase the risk of preterm delivery and giving birth to a low birth weight baby
- The oral cavity as a portal of nutrients for the body.
- The oral cavity for communication.
- Medical links between oral disease and other health entities.
- The importance of the oral cavity for self-esteem and social contacts.
Good physical and mental health are dependent upon the intake of healthy nutrients. The mouth is the initial part of the digestive system, health oral cavity is essential for the proper initial breakdown of the food as it enters the system. If the teeth and surrounding tissues are not healthy, general health is more at risk.
Communication is an essential part of daily living. Healthy teeth, healthy soft tissues and normal salivary function facilitate good speech.Good communication does not only mean the pronunciation of words and syllables but also facial expression and facial appearance – all part of a healthy and functional oral system.
In recent years, research has been looking into the direct connection between oral diseases and general health. Some of these connections are causal, where an oral disorder is related to the incidence of another systemic disorder, and some are concurrent, where people who are more likely to have one disease are also more likely to have an oral disorder at the same time.
The oral health/general health connection can come under any of the six following categories.
-
Oral conditions related to treatment for other systemic disorders.
Example – loss of salivary flow due to radiation treatment for head or neck cancer. This can cause increased tooth decay rates, loss of retention of dentures, or mouth discomfort.
-
Oral disease as a precursor of systemic disease.
Example – Leukoplakia (white patches) that develop into oral cancer and possibly metastasize to other areas.
-
Oral disorders as a marker of systemic disease.
Example – signs showing in the mouth may first detect conditions such as vitamin B12 deficiency, AIDS or diabetes.
-
Systemic disorders affecting oral tissues.
Example – Diabetes as a factor that reduces the body’s resistance to periodontal disease or other mucosal disorders.
-
Oral disorders affecting systemic conditions.
Examples – Periodontal disease as a possible causal factor or contributing factor for cardiovascular disease, pre-term low birth weight babies, aspiration pneumonia in the elderly, or other respiratory diseases.
-
Medical syndromes that affect the Oral Cavity as well as other parts of the body.
Example - Osteogenesis imperfecta, which affects the number or quality of teeth as well as the skeletal system.
All of the above oral health/general health connections or problems can be prevented, treated or ameliorated by being aware of their existence, paying attention to oral preventive home care and accessing professional oral health care.
In today’s world, the importance of good appearance and function of the oral cavity is much more important than in the past. Good oral health helps in socializing without embarrassment. Although it is not essential that everyone’s teeth appear the same, it is important for people to not have their teeth reflect negatively on them in their social contacts.
Despite the fact that dental care programs have been recommended in various health care programs in the past and in reports by governments, it appears that oral health is still by large considered outside the health care system and that more work needs to be done in demonstrating the connection between oral health and general health.
If you don't brush and floss regularly to keep your teeth clean, plaque can build up along your gum line, creating an environment for additional bacteria to accumulate in the space between your gums and your teeth causing gingivitis. When left untreated it could lead to periodontitis. The most severe form of gum infection is called acute necrotizing ulcerative gingivitis, also known as trench mouth.
Bacteria from your mouth normally does not enter your bloodstream. However, invasive dental treatments can provide a port of entry for these microbes. Medications or treatments that reduce saliva flow and antibiotics that disrupt the normal balance of bacteria in your mouth can also compromise your mouth's normal defenses, allowing these bacteria to enter your bloodstream.
If you have a healthy immune system, your immune system quickly dispenses with them, preventing infection. However, if your immune system is weakened because of a disease or cancer treatment, oral bacteria in your bloodstream (bacteremia) may cause you to develop an infection in another part of your body. In the case of Infective endocarditis, oral bacteria enter your bloodstream and stick to the lining of diseased heart valves.
The Indian government is committed to the care and wellbeing of its citizens which has paid off by adding years to the average life span. But not all Indians have benefitted from improvements in oral health and health care. Indian Dental Association (IDA) recognizes gaps in oral health and well-being which were revealed by the National Oral Health Survey. The weight of this gap is borne majorly by rural India. The Dentist Population ratio in rural India is dismally low with less than 2% dentists being available for 72% of the rural population. The grim reality in India is that 95% of the population suffers from gum disease, only 50% use a toothbrush and just 4.5 % of the population visit the dentist.
This survey served as a wake-up call to improve the oral health of the nation. It called upon policymakers, community leaders, private industry, health professionals, the media, and the public to affirm that oral health is essential to general health and well-being and a need to take action.
IDA’s immediate response was to address the ‘silent epidemic of oral diseases by initiating National Oral Health Programme(NOHP) which aims at optimal oral health for all.
Good oral health is vital to good overall health. Poor oral health negatively affects growth, development, learning, nutrition, communication and self-esteem for all sections of society; young and old; have and have-nots. Tooth decay is one of the most common chronic diseases.
IDA affirms that oral health is essential to general health and well-being and thus the need to take action. IDA aims that
- Nobody suffers from oral diseases which can be prevented and treated.
- Young children should not suffer from caries.
- Rural populations should not experience poor oral health due to barriers to access to care, resources and professionals.
IDA call-for-action accurately assesses needs, monitors outcomes, decreases disparities, improves access to care and ultimately improves oral health.
- Oral health being more than just healthy teeth.
- Oral diseases and disorders affecting health and well-being throughout life.
- The mouth reflecting general health and well-being.
- Lifestyle behaviours (tobacco use, excessive alcohol use and poor dietary choices) affecting oral and craniofacial health.
- Safe and effective measures existing to prevent—dental caries and periodontal diseases.
- Information needed to improve India’s oral health and eliminate health disparities.
Knowledge and tools of the 21st century provide a new window into the complex link between oral health and general health. Science is advancing rapidly and breakthroughs in oral, dental and craniofacial research prove that oral diseases, such as caries, periodontal disease, oral cancers and sports-related injuries of the craniofacial complex are all preventable.
We conclude that the morbidity, mortality and economic burden associated with these conditions can be considerably reduced by programs and interventions aimed at prevention and health promotion.
Oral diseases are progressive, cumulative and become more complex over time. They can affect our ability to eat, how we look and the way we communicate. Healthy teeth help a child to eat properly, speak clearly and guide adult teeth into place. Good oral health helps seniors get proper nutrition, maintain good overall health and enjoy a better quality of life.
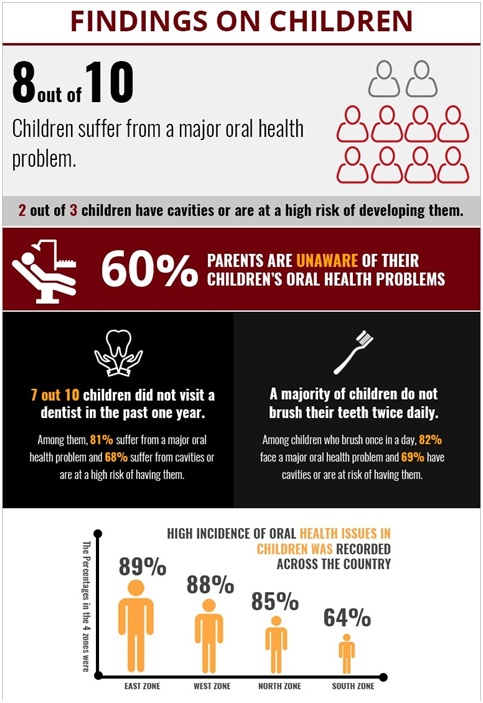
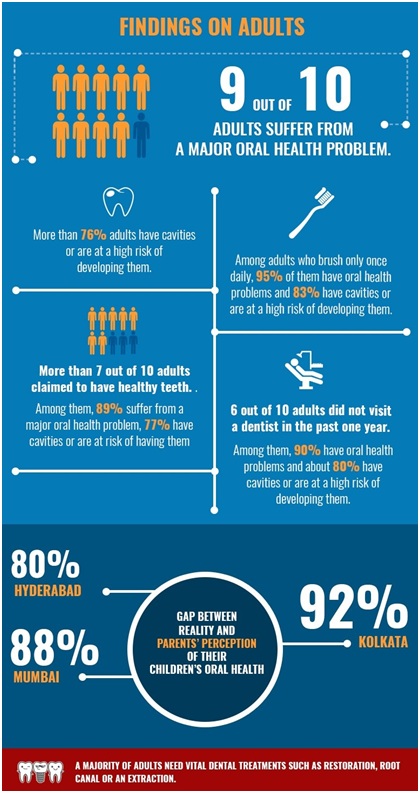
The following are highlights of oral health data for children and adults.
This is the inspiration to build a stronger, more effective and efficient oral health care system that would contribute to the health and well-being of all Indians. Initiatives by IDA enhance oral health and by enlisting the expertise of dental professions, individuals, health care providers, communities and policymakers at all levels of society.
The Wake-up Call To Action is
- for optimal oral health, acknowledging oral health is a fundamental part of general health and well-being.
- engage in programmes to promote oral health and prevent disease.
of the Call To Action is to
- promote oral health.
- improve the quality of life.
- eliminate oral health disparities.
As a force for change to enhance the nation’s overall health and well-being, IDA urges that oral health promotion, disease prevention and oral health care has a presence in all health policy agendas set at local, state and national levels. In addition, IDA seeks to address the nation’s overall health agenda.
The perception ingrained in Indian mindset is that o
ral health is less important than and separate from general health. Activities to overcome these attitudes and beliefs must be taken up at grassroots level by oral health literacy, basic oral and craniofacial information. This will help promote the general health and well-being of all Indians.
Change public perceptions
- Enhance oral health literacy
- Develop messages that are culturally sensitive and linguistically competent.
- Enhance knowledge of the value of regular, professional oral health care.
- Increase the understanding of how oral infections can indicate general health status.
Change policymakers’ perceptions
- Inform government of the results of oral health research and programmes.
- Develop concise and relevant messages for the government.
- Document the health and quality-of-life outcomes.
Change dentists’ perceptions
- Review and update dentists via CE courses
- Train dentists to conduct oral screenings.
- Promote interdisciplinary training of dental personnel.
- Encourage dentist’s to refer patients to other health specialists.
Reduce disease and disability through education, behavioural change, risk reduction, early diagnosis and disease prevention management.
Improve oral health care access by addressing poverty, education or language skills, geographic isolation, age, gender, disability, or an existing medical condition.
Enhance health promotion and health literacy by healthier lifestyles and interventions for prevention by tobacco cessation, dietary choices, wearing protective gear for sports. Many Indians do not realize the importance of oral health and preventive measures. Therefore :
Identify and reduce disease and disability
- Implement science-based interventions.
- Enhance oral health-related content in health professions school curricula.
- Build and support epidemiologic and surveillance databases.
- Data on oral health status, disease and health services.
- Encourage partnerships by organizing workshops and conferences.
Improve access to oral health care
- Promote and execute programmes.
- Create an active and up-to-date database.
- Explore policy changes and enhance patient access to care.
- Remove barriers to the use of services.
- Assist low-income patients.
- Facilitate health insurance.
- Energize and empower the public.
- Develop integrated and comprehensive care programmes.
Advances in health depend on biomedical and behavioural research aiming at understanding the causes and pathological processes of diseases. This will lead to interventions that will improve prevention, diagnosis and treatment. Of importance is oral health research on chronic oral infections associated with heart and lung disease, diabetes, and premature low birth-weight babies. Hybrid sciences, for example, bio-engineering studies are establishing the basis for repair and regeneration of the body’s tissues and organs—including teeth, bones, and joints-- and ultimately full restoration of function. Oral diagnostics, using saliva or oral tissue samples, will contribute to overall health surveillance and monitoring. Efforts are needed to transfer new oral knowledge into improved means of diagnosis, treatment, and prevention. The public needs to be informed, accurately and often, of findings that affect their health.
Meet patient needs. The provider can play a catalytic role as a community spokesperson, addressing key health problems and service needs. While the number of women engaged in the health professions is increasing, the number of underrepresented racial and ethnic minorities is decreasing and remains limited. Enhance oral health workforce capacity. Dental school recruitment programmes must offer incentives to students to practice in rural areas and inner cities. To effect change in oral health workforce capacity, more training and recruitment efforts are needed. Currently, there is a crisis to recruit clinicians into research careers. Efforts are underway to address these needs, but the rate of recruitment and retention is slow.
Efforts are needed to:
- Change the racial and ethnic composition of the workforce
- Document the outcomes of existing efforts.
- Expand and build upon successful recruitment and retention programmes.
- Inform and encourage individuals to pursue health and science career options.
Ensure a sufficient workforce pool to meet health care needs by
- Expand scholarships and loan repayment efforts at all levels.
- Specify and identify resources for conducting outreach and recruitment.
- Develop mentoring programmes to ensure the retention of individuals.
- Provide training in communication skills and cultural competence.
Secure an adequate and flexible workforce by:
- Assess the existing capacity and distribution of the oral health workforce.
- Extend or expand workforce capacity to address oral health care in remote areas.
- Ensure oral health expertise availability to health and government programmes.
The private sector and public sector each has unique characteristics and strengths. Linking the two can result in a creative synergy capitalizing on the talent and resources of each partner. the , efforts are needed within each sector to increase the capacity for programme development, for building partnerships, and for leveraging programmes. A sustained effort is needed right now to build the nation’s oral health infrastructure to ensure that all sectors of society--the public, private practitioners, and government personnel--have sufficient knowledge, expertise, and resources to design, implement and monitor oral health programmes. Most importantly, the public in the form of voluntary organizations, community groups, or as individuals, must be included in any partnership that addresses oral and general health.
Successful partnering at all levels of society will require efforts to:
- Strengthen the networking capacity to address oral health needs.
- Build and nurture broad-based coalitions.
- Strengthen collaborations among dental, medical, and public health communities for research, education, care delivery, and policy development.
- Develop partnerships that are community-based, cross-disciplinary, and culturally sensitive.
- Work with the Partnership Network and other coalitions to address the four actions previously described: change perceptions, overcome barriers, build a balanced science base, and increase oral health workforce diversity, capacity, and flexibility.
This action plan will serve as a blueprint, one that can be a tool for enlisting collaborators and partners. Building this plan into existing health programmes will maximize the integration of oral health into general health programmes—not only by incorporating the expertise of multidisciplinary professional teams, but also allowing the plan to benefit from economies of scale by adding on to existing facilities, utilizing existing data and management systems and serve the public.
- Your teeth are sensitiveto hot or cold
- Your gums are puffy and/or they bleedwhen you brush or floss
- You have fillings, crowns, dental implants, or dentures
- You don’t like the way your smile or teeth look
- You have persistent bad breathor a bad taste in your mouth
- You are pregnant
- You have pain or swelling in your mouth, face or neck
- You have difficulty chewing or swallowing
- You have a family history of gum diseaseor tooth decay
- You have a medical condition such as diabetes, cardiovascular disease, eating disorders, or are HIV positive
- Your mouth is often dry
- You smokeor use other tobacco products
- You are undergoing medical treatment such as radiation, chemotherapy or hormone replacement therapy
- Your jawsometimes pops or is painful when opening and closing, chewing or when you first wake up; you have an uneven bite
- You have a spot or sorethat doesn’t look or feel right in your mouth and it isn’t going away.
The IDA Dental Symptom Checker can help you understand what your dental symptoms may mean so that you can make informed decisions about your dental health.